Corneal Transplants
The cornea is the outer most portion of the eye which helps you see clearly. Made up of five layers, the cornea is quite strong and serves as the eye’s first defense against damage to the rest of the eye. While durable, the cornea is highly sensitive and susceptible to injury and diseases like keratoconus. While the cornea can repair itself after many injuries and diseases without surgery, those left untreated or more traumatic corneal injuries can lead to the need for a corneal transplant.
About Corneal Transplant Surgery
Typically, surgery is reserved for those suffering from severe corneal scarring, Fuchs’ Dystrophy and as a form of keratoconus treatment. Corneal transplants are considered when all other options have been exhausted, and eyeglasses and contact lenses are no longer a viable way to correct vision. While a last resort, however, corneal transplants are frequently performed in the United States with estimates of about 50,000 performed each year according to the National Eye Institute. The chances of success for this operation have risen dramatically because of technological advances. Corneal transplantation has restored sight to many, who a generation ago would have been blinded permanently by corneal eye disease, injury, infection, or inherited disease or degeneration.
 Generally, patients are unaware of what is impacting their vision until they meet with their eye doctor who then refers them to a specialist. Wolfe Eye Clinic cornea specialists are frequently referred to by optometrists across Iowa for our corneal eye disease expertise and premier care. In 1960, Wolfe Eye Clinic surgeons began performing corneal transplants which had previously been performed exclusively in University settings. Having performed thousands of corneal transplant surgeries, Wolfe Eye Clinic cornea specialists are experts in restoring vision. While the thought of corneal transplant surgery can be overwhelming, your Wolfe Eye Clinic cornea surgeon and our experienced teams are with you every step of the way.
Generally, patients are unaware of what is impacting their vision until they meet with their eye doctor who then refers them to a specialist. Wolfe Eye Clinic cornea specialists are frequently referred to by optometrists across Iowa for our corneal eye disease expertise and premier care. In 1960, Wolfe Eye Clinic surgeons began performing corneal transplants which had previously been performed exclusively in University settings. Having performed thousands of corneal transplant surgeries, Wolfe Eye Clinic cornea specialists are experts in restoring vision. While the thought of corneal transplant surgery can be overwhelming, your Wolfe Eye Clinic cornea surgeon and our experienced teams are with you every step of the way.
How does a corneal transplant work?
 In corneal transplant surgery, the cornea surgeon removes a portion of the cornea and replaces it with a clear, healthy cornea, donated through an eye bank. Wolfe Eye Clinic works closely with Iowa Lions Eye Bank to receive preserved healthy corneas that were graciously donated post-mortem by deceased individuals registered as organ donors. There are three main types of corneal transplants differentiated by how many of the cornea’s five layers need to be transplanted: penetrating keratoplasty (full thickness), lamellar keratoplasty (outer layers) and endothelial keratoplasty (inner layers).
In corneal transplant surgery, the cornea surgeon removes a portion of the cornea and replaces it with a clear, healthy cornea, donated through an eye bank. Wolfe Eye Clinic works closely with Iowa Lions Eye Bank to receive preserved healthy corneas that were graciously donated post-mortem by deceased individuals registered as organ donors. There are three main types of corneal transplants differentiated by how many of the cornea’s five layers need to be transplanted: penetrating keratoplasty (full thickness), lamellar keratoplasty (outer layers) and endothelial keratoplasty (inner layers).
During corneal transplant surgery, anesthesia is used and patients are given topical eye drops to help increase comfort. Corneal transplant surgeries are performed at Wolfe Eye Clinic’s Des Moines and Hiawatha (Cedar Rapids) surgical centers on an out-patient basis, meaning you are not required to stay overnight at our facilities. Following surgery, pain is usually mild for the first week and patients’ vision may be blurry for a period of time. The length of time it takes to see an improvement in vision and fully recover from a corneal transplant depends on the type of corneal transplant surgery performed. This can range from one month to one year. Common side effects that patients report after surgery are a foreign body sensation, scratchiness and blurriness. Your cornea specialist at Wolfe Eye Clinic will be there for you with any questions you may have about your recovery.
Types of Corneal Transplants
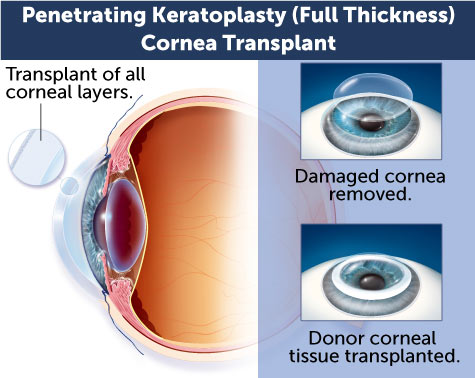
Penetrating Keratoplasty (Full Thickness) Cornea Transplant
Penetrating keratoplasty involves transplanting all layers of the cornea from the donor (full thickness). During penetrating keratoplasty, a circular button-shaped section of corneal tissue is removed from the diseased or damaged cornea. A matching button-shaped section of corneal tissue from the donor is then positioned and sutured into place. Following surgery, stitches are progressively removed about every six weeks and healing can take up to a year. Occasionally, a Laser Assisted Keratoplasty (LAK) utilizes a femtosecond laser at the eye bank to create a custom sized transplant for an individual patient.
Deep Anterior Lamellar Keratoplasty (DALK) Cornea Transplant
Deep Anterior Lamellar Keratoplasty is a cornea transplant procedure where the outermost layers of the cornea are replaced. This procedure can be used to treat deep anterior corneal abrasions and as a form of keratoconus treatment. There is preservation of the recipient patient's own endothelial cells possibly making rejection episodes less likely.
Endothelial Keratoplasty Cornea Transplant
Endothelial keratoplasty, also known as EK, replaces only the innermost layer of the cornea called the endothelium layer and leaves the overlying healthy corneal tissue intact. For patients with disorders involving the innermost layer of the cornea, EK is the procedure of choice. With this method, the surgeon makes a tiny incision and places a thin disc of donor tissue on the back surface of the cornea. An air bubble is used to position the new layer into place. The small incision is self-sealing and typically no sutures are required.
Endothelial keratoplasty has several advantages over full-thickness penetrating keratoplasty. These include faster recovery of vision, minimal removal of corneal tissue, no related complications with sutures, and reduced risk of astigmatism, or an asymmetrically shaped cornea, after surgery.
The most common disease treated with this condition is Fuchs Endothelial Dystrophy (FED). Fuchs Dystrophy leads to a progressive loss of endothelial cells over time. Loss of these delicate cells can lead to corneal swelling known as corneal edema and cause the cornea to cloud. Seventy five percent of the corneal transplants performed at Wolfe Eye Clinic are of the endothelial keratoplasty variety. There are two versions of endothelial keratoplasty corneal transplant surgery:
Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) & Descemet's Membrane Endothelial Keratosplaty (DMEK).
Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) & Descemet's Membrane Endothelial Keratosplaty (DMEK)
With both DSAEK and DMEK surgeries, an air bubble is used to secure the cornea within the eye after transplantation. Both surgeries require patients to lay on their back for a period of time following surgery. Not everyone is a candidate for these surgeries, and rest assured your corneal surgeon will discuss with you which corneal transplant option is most beneficial for you and answer any questions you may have.
How successful are corneal transplants?
As technology has advanced, the success of corneal transplants has as well. There are still significant risks, but the risk of complications varies depending on how many layers of the cornea are transplanted. Complications can include the body rejecting the donor corneal tissue (cornea graft rejection), eye infection, and problems associated with the use of sutures.
Fortunately, cornea graft rejection is a rare event, especially with endothelial keratoplasty. Transplant rejection occurs when the body’s immune system detects the donor cornea as a foreign body and reacts to it. Rejection signs may occur as early as one month or as late as several years after surgery. The surgeon will prescribe medication that can help prevent the rejection process. Should a transplant fail, corneal transplant surgery can be repeated.
Contact the Iowa Cornea Surgeons at Wolfe Eye Clinic
Wolfe Eye Clinic corneal specialists treat corneal injuries and corneal diseases throughout Iowa, including Ankeny, Des Moines, Fort Dodge, Hiawatha (Cedar Rapids), Iowa City, Marshalltown, Ottumwa and Pleasant Hill. If you have questions or would like to schedule an appointment with one of our corneal disease specialists, fill out our form here, or give us a call at (833) 474-5850.